In recent years, with the increasing number of obesity cases, there has also been a significant increase in the number of bariatric surgeries. Among these surgeries, the gastric sleeve is one of the most frequently performed.
Gastric sleeve surgery is a very common procedure, but is it without risks? Isn’t it dangerous? Of course, as with all surgical procedures, this procedure carries risks, both specific to general surgery and those specific to this procedure.
These risks can be divided into two main categories: immediate and long-term.
The most important risks among early maturity risks are bleeding and leakage risks.
-Bleeding risk: During the operation, the stomach is reduced, and a stapler, colloquially known as a stapler, is used for this purpose. These lines are checked during and after the operation, and the operation is generally concluded after ensuring that there is no bleeding. However, if bleeding from a capillary vessel occurs in the first hours after the operation (the first 24-36 hours), this is called “hemorrhage.” If it exceeds a certain level and does not stop on its own, it can reach dangerous levels. In such cases, depending on the extent of the problem, the patient may be admitted for surgery again, or the patient may be referred for surgery again depending on the severity of the condition. The risk of bleeding after this operation is around 1-2%.
-Leak risk: When a problem, an opening, a break, or a leak occurs in the staple line we just mentioned, this is called a leak. Even if the risk of a leak is 1% or lower, it can cause serious illness and reach dangerous levels if it develops. Leaks are usually checked during the operation. However, this is of no significance. The main cause of leaks is tissue blood flow and oxygen problems. The primary cause of low oxygen supply to the tissue can be zigzags in the staple lines. When oxygen is insufficient, the tissue wears out and can lead to a leak in the staple line. This usually occurs within 7-14 days. Therefore, during Sleeve Gastrectomy surgery, patients are given only liquids for the first two weeks to prevent excessive pressure on the staple line. In other procedures, pureed foods are offered for the first two weeks because the risk of leaks is lower.

Among the long-term risks, the most important ones are stomach stenosis, rotation or gastric sleeve herniation, gallbladder stones, and reflux.
Stomach twist or inversion: The stomach rotates on its axis after a certain period of time. This can usually occur within a few months, typically within the first 2-3 years. One of the most important causes of inversion is the unevenness of the front and back surfaces of the stomach. Furthermore, changes resulting from tissue healing can also cause this. When inversion occurs, the patient experiences problems with food intake. The patient may even vomit frequently. The usual solution is a revisional, or inversion, operation. The RNY Gastric Bypass Surgery is generally the most preferred method in these operations.
-Stomach stenosis: One of the effects of the aforementioned gastric torsion is a narrowing of the stomach passage. Furthermore, if the stomach is initially too narrow, it can become even narrower over time as the tissue heals, causing serious difficulties in passing food. In the case of a sleeve gastrectomy, the location of the stenosis is important. If the stenosis is in the upper regions, the solution is difficult. If the stenosis is in the lower regions, which is usually the case, the procedure can be converted to gastric bypass surgery to relieve the narrowed area.
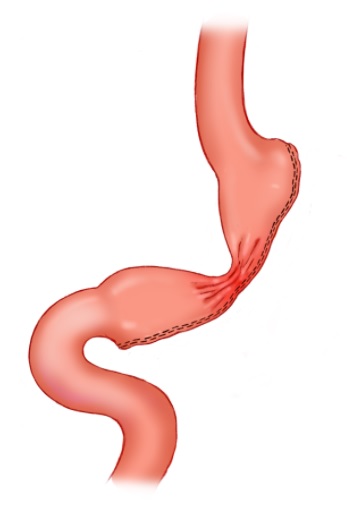
-Gastric Sleeve Herniation: This is the term given to the partial displacement of the gastric sleeve into the thorax, or rib cage. A herniation can occur after a gastric sleeve procedure in people prone to a gastric hernia. Therefore, a gastric sleeve procedure is not recommended for those with a gastric hernia or severe reflux prior to the procedure.
-Gastric Reflux: According to research, this condition can occur in 30% of patients. While it can be quite uncomfortable, it may require gastric protective medications. It generally occurs in those who have had reflux prior to the procedure, and therefore, a gastric sleeve procedure is not recommended for those with obvious reflux prior to the procedure. If the reflux is severe, a revision surgery, that is, a conversion to another procedure, may be necessary to address the issue.
Gallstones: This condition can occur in 10% of patients within 1-2 years. Factors such as low fluid intake, rapid weight loss, and genetic predisposition can contribute to the condition. It can be detected with an ultrasound and necessitate gallbladder surgery, which is considered a relatively straightforward procedure.
Of course, in addition to these complications, we can also list the complications that can occur with any type of surgery: incisional hernia, wound infection, and embolism (clotting). While embolism is extremely rare, it can be very dangerous when it occurs.

